Maveryx Success Stories
Learn how Alteryx customers transform their organizations using data and analytics.STORIES WANTED
Showcase your achievements in the Maveryx Community by submitting a Success Story now!
SUBMISSION INSTRUCTIONS- Community
- :
- Community
- :
- Learn
- :
- Success Stories
- :
- Enhancing Epic Reporting with Alteryx
Enhancing Epic Reporting with Alteryx
- Subscribe to RSS Feed
- Mark as New
- Mark as Read
- Bookmark
- Subscribe
- Printer Friendly Page
- Notify Moderator
Overview of Use Case
The Analytics and Data Innovations team at an American healthcare provider used Alteryx to assess quality measures for reporting to The Joint Commission and Centers for Medicare and Medicaid Services. Prior to Alteryx, it was not possible to augment reporting due to limitations in file size and reliance on manual processes. Within two weeks of using Alteryx, the team was able to enhance reporting capabilities, saving about 200 hours each month to focus on quality improvement efforts.
Our team was tasked with developing reporting on quality measures for quarterly reports shared with The Joint Commission (TJC) and Centers for Medicare and Medicaid Services (CMS). These agencies evaluate hospitals and healthcare providers on core measures based on nationwide standards and recognize top performers for key quality metrics and accreditation, something very important to our Executive leadership.
We had been struggling to produce comprehensive reports due to platform restrictions limiting the amount of data included. We could produce a file for the third-party reporting tool but it was time intensive and lacked the ability to supplement more data tables to our file. It became evident that we needed to find an alternative solution and that’s when we turned to Alteryx.
As a leading healthcare provider, data is crucial for the success of our organization. Our ADI team is responsible for supporting several different initiatives and we provide functional teams with the data and insights needed to deliver the best outcomes for the business. Having worked as a healthcare data analyst for the last ten years, I’ve used a variety of tools to extract data from Epic databases, but nothing has come close to Alteryx
Prior to Alteryx, our process included extracting data from Epic, pulling in information like patient demographics, inpatient diagnosis, and quality reports. The data was then formatted and organized before an output file was uploaded to Premier, a third-party tool used for reporting to CMS and TJC. While the current process was working, our team was unable to supplement additional information needed to achieve better results.
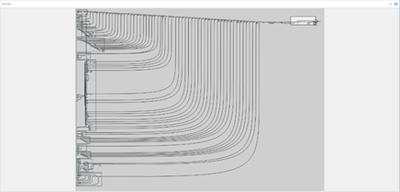
Alteryx totally changed the way I managed our reporting data. Designer was mentioned by a new manager when he joined our team but it wasn't adopted for a few months until I had exhausted all other options. The first time I ran our previous process in Designer it took around 7 minutes, down from 8 hours. This is when I realized the power of Alteryx. The added efficiencies allowed the reporting tool to include more information, faster than before, letting the team spend more time on improvements in patient outcomes. Since then, I've tripled the amount of information outputted in our file and automated the workflow using Server, something we never could have done without Alteryx. We now have a comprehensive workflow, which can easily be modified and altered depending on the criteria of our tasks.
-
Adobe
2 -
Alteryx Connect
5 -
Alteryx Designer
202 -
Alteryx for Good
1 -
Alteryx Promote
2 -
Alteryx Server
66 -
Alteryx using Alteryx
29 -
Americas
158 -
Analyst
108 -
Analytics Leader
54 -
Asia Pacific
29 -
AWS
9 -
BI + Analytics + Data Science
100 -
Business Leader
37 -
C-Leader
18 -
Data Prep + Analytics
230 -
Data Science + Machine Learning
113 -
Data Scientist
14 -
Department: Other
14 -
Education
18 -
Energy + Utilities
5 -
Europe + Middle East + Africa
58 -
Experian
2 -
finance
29 -
Financial Services
33 -
Healthcare + Insurance
21 -
Human Resources
19 -
Information Technology
25 -
IT
31 -
Life Sciences + Pharmaceuticals
3 -
Manufacturing
20 -
Marketing
16 -
Media + Entertainment
12 -
Microsoft
52 -
Operations
38 -
Other
10 -
Process Automation
59 -
Professional Services
69 -
Public Sector
15 -
Qlik
1 -
Retail + CPG
32 -
Sales and Service
24 -
Salesforce
9 -
SAP
11 -
Snowflake
6 -
Tableau
71 -
Tech Partner: Other
86 -
Technology
34 -
Telecommunications
5 -
Teradata
5 -
Thomson Reuters
1 -
Transportation + Logistics
25 -
Travel + Hospitality
4 -
UiPath
1
- « Previous
- Next »